- 0086-571-85302990
- sales@greenskybio.com
From Remedies to Science: Understanding the Antibacterial Properties of Plant Extracts
2024-07-18
1. Introduction
Plants have been an integral part of human health care for centuries. Antibacterial properties of plant extracts have been utilized in traditional remedies across different cultures. However, the journey from these traditional uses to scientific understanding has been a long and fascinating one. This article aims to explore this transformation, highlighting the historical use of plants for treating infections and the modern scientific investigations into the mechanisms underlying their antibacterial actions.
2. Historical Use of Plants as Antibacterial Remedies
2.1 Ancient Civilizations
Ancient civilizations such as the Egyptians, Greeks, and Chinese had extensive knowledge of using plants for medicinal purposes. For example, the Egyptians used myrrh and frankincense in embalming processes, which also had antibacterial properties that helped preserve the body. The Greeks, led by Hippocrates, were known to use plants like thyme and sage to treat various ailments, some of which were likely due to bacterial infections. In China, traditional medicine has a long history of using plants such as ginger and garlic for their health - promoting and antibacterial effects.
2.2 Indigenous Cultures
Indigenous cultures around the world also had their own unique plant - based remedies. Native American tribes, for instance, used echinacea to boost the immune system and fight off infections. In Africa, the neem tree has been used for centuries for its antibacterial, antifungal, and antiviral properties. These traditional uses were often passed down through generations orally, and were based on empirical observations of the effects of plants on human health.
3. Modern Scientific Exploration of Plant Extracts' Antibacterial Properties
3.1 Identification of Active Compounds
With the development of modern scientific techniques, researchers have been able to identify the active compounds in plant extracts that are responsible for their antibacterial properties. For example, flavonoids are a group of compounds found in many plants such as tea and apples that have been shown to have antibacterial activity. Alkaloids in plants like cinchona (the source of quinine) also exhibit antibacterial effects. Scientists use techniques such as chromatography and spectroscopy to isolate and identify these compounds.
3.2 Mechanisms of Action
Understanding how these plant - derived compounds act against bacteria is crucial. Some plant extracts work by disrupting the bacterial cell wall. For instance, lysozyme - like substances in certain plant extracts can break down the peptidoglycan layer in the cell wall of bacteria, leading to cell lysis. Others may interfere with bacterial protein synthesis. Compounds like tetracycline - like substances from plants can bind to the bacterial ribosomes and prevent the synthesis of essential proteins. Additionally, some plant extracts can affect the bacterial cell membrane, altering its permeability and causing leakage of intracellular components.
4. In - vitro and In - vivo Studies
4.1 In - vitro Studies
In - vitro studies are often the first step in evaluating the antibacterial properties of plant extracts. These studies involve testing the extracts against bacterial cultures in a laboratory setting. Researchers can determine the minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) of the extracts. For example, a study might test different concentrations of a Lavender Extract against Staphylococcus aureus bacteria. By observing the growth of the bacteria in the presence of the extract at various concentrations, the MIC and MBC can be determined, which gives an indication of the potency of the extract.
4.2 In - vivo Studies
While in - vitro studies provide valuable initial information, in - vivo studies are necessary to understand the real - world effectiveness of plant extracts. In - vivo studies involve testing the extracts in living organisms, such as animals or humans. However, conducting in - vivo human studies is more complex due to ethical considerations and regulatory requirements. Animal models are often used first. For example, a study might test the antibacterial effect of a turmeric extract on mice infected with a particular bacterial pathogen. The results from these animal studies can then be used to inform potential human trials.
5. Potential Applications of Plant Extracts in Antibacterial Therapy
5.1 Complementary and Alternative Medicine
In the field of complementary and alternative medicine, plant extracts have a significant role. Many people prefer to use natural products for minor infections or as preventive measures. For example, oregano oil, which has strong antibacterial properties, is often used as a natural alternative to antibiotics for treating minor respiratory or gastrointestinal infections. These plant - based remedies can also be used in combination with conventional medicine in some cases.
5.2 Drug Development
Plant extracts can also serve as a source of new antibacterial drugs. Pharmaceutical companies are increasingly interested in screening plant extracts for potential drug candidates. The active compounds identified in plants can be further modified and optimized to develop more effective and safer antibacterial drugs. For example, the development of new drugs based on the structure of artemisinin, a compound from the Artemisia annua plant, which has been used in the treatment of malaria, shows the potential of plant - derived compounds in drug development.
6. Challenges and Limitations
6.1 Standardization
One of the major challenges in using plant extracts for antibacterial purposes is standardization. The composition of plant extracts can vary depending on factors such as the plant species, growth conditions, and extraction methods. This variability makes it difficult to ensure consistent antibacterial activity. For example, the concentration of active compounds in an aloe vera extract can differ significantly depending on where the plant was grown and how it was processed.
6.2 Toxicity
Although plant extracts are generally considered natural, some may still have toxicity issues. High doses of certain plant extracts can cause adverse effects in the body. For example, comfrey contains pyrrolizidine alkaloids, which can be toxic to the liver if consumed in large amounts. Therefore, it is important to carefully evaluate the safety of plant extracts before using them for antibacterial therapy.
7. Conclusion
The study of the antibacterial properties of plant extracts has come a long way from traditional remedies to modern scientific exploration. Understanding the historical use of plants in treating infections provides a foundation for modern research. The identification of active compounds and the elucidation of their mechanisms of action open up new possibilities for the development of antibacterial therapies. However, challenges such as standardization and toxicity need to be addressed. Overall, plant extracts hold great potential in the fight against bacteria, and continued research in this area will benefit both traditional medicine enthusiasts and scientific researchers alike.
FAQ:
What are some historical uses of plant extracts for treating infections?
Throughout history, plant extracts have been used in various ways to treat infections. For example, certain herbs were made into poultices and applied directly to wounds. Some plants were brewed into teas to be consumed for internal infections. Willow bark, which contains salicin (a precursor to aspirin), was used for its anti - inflammatory properties which also had implications in fighting off certain infections related to inflammation. Another example is garlic, which has been used for centuries in different cultures for its antimicrobial properties, often used to treat gastrointestinal infections.
How does modern science study the antibacterial properties of plant extracts?
Modern science uses a variety of techniques to study the antibacterial properties of plant extracts. Laboratory tests such as in - vitro assays are commonly employed. In these assays, plant extracts are exposed to different types of bacteria in a controlled environment, and the growth inhibition of the bacteria is measured. Scientists also use techniques like chromatography to isolate and identify the active compounds within the plant extracts. Additionally, genetic analysis can be used to study how the bacteria respond at the molecular level to the exposure to plant extracts, which helps in understanding the mechanisms of action.
What are the main challenges in turning plant - based remedies into scientific antibacterial treatments?
One of the main challenges is standardization. The composition of plant extracts can vary depending on factors such as the plant's origin, growth conditions, and the extraction method used. Another challenge is ensuring consistent efficacy. While traditional use may suggest effectiveness, it can be difficult to reproduce the same results in a scientific setting. There are also regulatory hurdles to overcome. Developing plant - based antibacterial treatments requires meeting strict regulatory requirements for safety and efficacy, which can be complex and time - consuming. Additionally, understanding the long - term effects of these plant - based treatments on human health and the environment is also a concern.
Can plant extracts replace conventional antibiotics?
At present, it is unlikely that plant extracts can completely replace conventional antibiotics. While plant extracts show antibacterial properties, the effectiveness of antibiotics in treating severe and life - threatening bacterial infections is well - established. However, plant extracts can play an important complementary role. They may be useful in cases where antibiotic resistance is a concern, as they can offer alternative mechanisms of action against bacteria. Also, in milder infections or as part of preventive health measures, plant extracts could potentially be used.
What are some of the most promising plant extracts in terms of antibacterial properties?
Tea tree oil is one of the well - known plant extracts with strong antibacterial properties. It has been shown to be effective against a wide range of bacteria, especially those associated with skin infections. Oregano oil is also very promising, containing compounds like carvacrol and thymol which have antibacterial activity. Echinacea Extracts have been studied for their potential antibacterial effects, particularly in relation to respiratory infections. And turmeric extract, with its active compound Curcumin, has shown antibacterial properties as well, especially against some food - borne pathogens.
Related literature
- Antibacterial Activity of Plant Extracts: A Review"
- "The Science Behind the Antibacterial Properties of Traditional Medicinal Plants"
- "Plant Extracts as a Source of New Antibacterial Agents: Current Status and Future Perspectives"
- ▶ Hesperidin
- ▶ Citrus Bioflavonoids
- ▶ Plant Extract
- ▶ lycopene
- ▶ Diosmin
- ▶ Grape seed extract
- ▶ Sea buckthorn Juice Powder
- ▶ Fruit Juice Powder
- ▶ Hops Extract
- ▶ Artichoke Extract
- ▶ Mushroom extract
- ▶ Astaxanthin
- ▶ Green Tea Extract
- ▶ Curcumin
- ▶ Horse Chestnut Extract
- ▶ Other Product
- ▶ Boswellia Serrata Extract
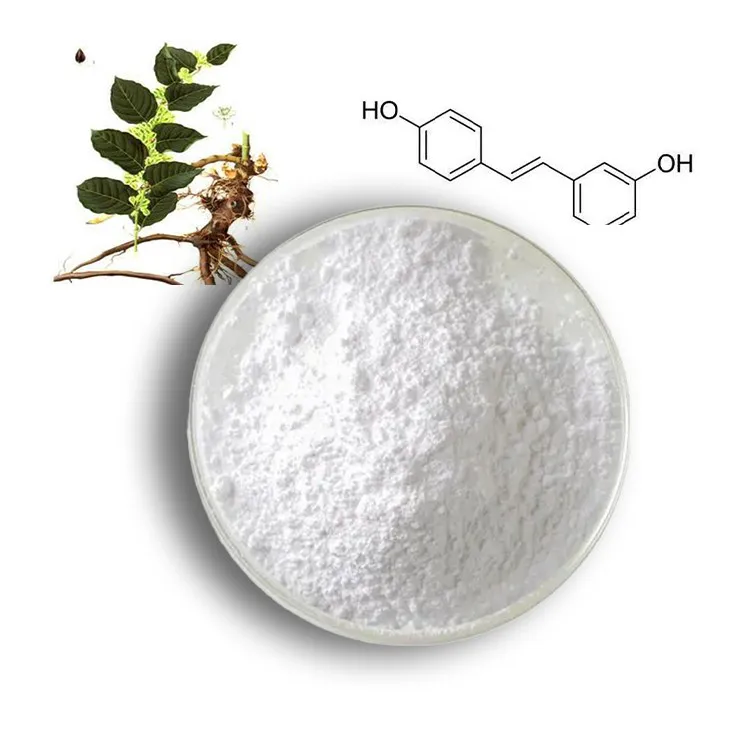
- ▶ Resveratrol
- ▶ Marigold Extract
- ▶ Grape Leaf Extract
- ▶ New Product
- ▶ Aminolevulinic acid
- ▶ Cranberry Extract
- ▶ Red Yeast Rice
- ▶ Red Wine Extract
-
Camu Camu Extract
2024-07-18
-
Lemon Balm Extract
2024-07-18
-
Resveratrol extract
2024-07-18
-
Echinacea Extract
2024-07-18
-
Lavender Extract
2024-07-18
-
Senna Leaf Extract
2024-07-18
-
Berberis aristata Extract
2024-07-18
-
Artichoke Leaf Extract
2024-07-18
-
Withania Somnifera Extract
2024-07-18
-
Black Pepper Extract
2024-07-18