- 0086-571-85302990
- sales@greenskybio.com
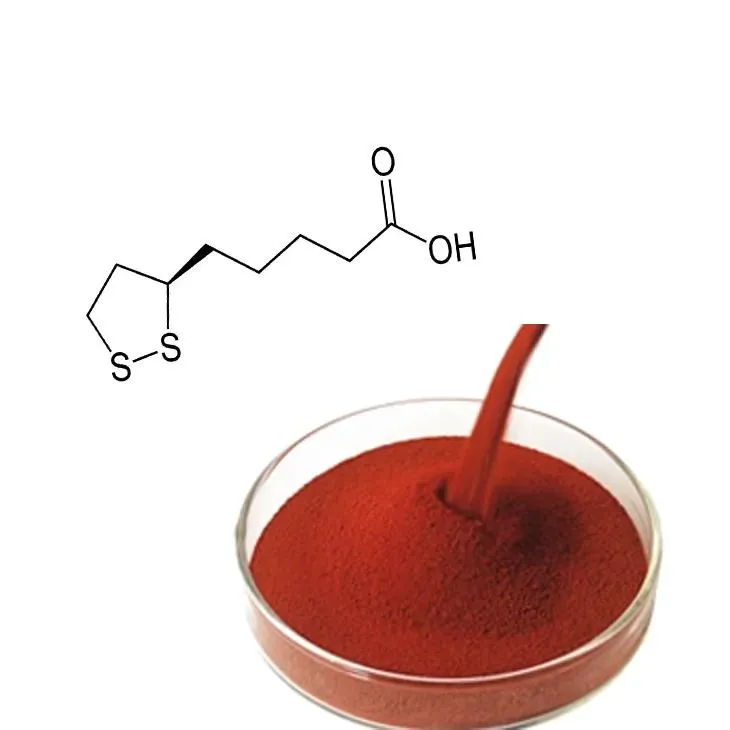
The optimal bioavailability of shikonin.
2024-12-01

1. Introduction
Shikonin, a natural naphthoquinone compound, has attracted significant attention in the field of medicine due to its diverse biological activities. These include anti - inflammatory, antibacterial, antitumor, and antioxidant properties. However, the full - scale application of Shikonin in clinical settings has been hampered by its relatively low bioavailability. Bioavailability refers to the fraction of an administered drug that reaches the systemic circulation in an active form and is available at the site of action. Understanding and optimizing the bioavailability of Shikonin is crucial for maximizing its therapeutic potential.

2. Chemical structure and its influence on bioavailability
The chemical structure of shikonin plays a fundamental role in determining its bioavailability. Shikonin has a lipophilic naphthoquinone core, which affects its solubility and permeability across biological membranes.
2.1 Solubility
The lipophilic nature of shikonin makes it poorly soluble in aqueous solutions. Low solubility can limit its dissolution in the gastrointestinal tract, thereby reducing the amount available for absorption. Strategies to enhance solubility include the formation of prodrugs, which are modified forms of the drug that can be more easily dissolved and then converted back to the active form in the body. Another approach is the use of nanoparticle - based formulations, where shikonin is encapsulated within nanoparticles to improve its solubility.
2.2 Permeability
Despite its lipophilicity, shikonin may face challenges in permeating certain biological membranes. The presence of polar groups in its structure can interact with membrane components in ways that impede its passage. Modifying the structure to optimize the balance between lipophilicity and hydrophilicity can potentially enhance permeability. For example, the addition of certain functional groups that can interact more favorably with membrane transporters may increase the rate of shikonin's passage across membranes.

3. Absorption of shikonin
The absorption of shikonin is a complex process that is influenced by multiple factors.
3.1 Gastrointestinal absorption
In the gastrointestinal (GI) tract, shikonin absorption is affected by the pH environment. The acidic pH of the stomach and the alkaline pH of the intestines can impact its chemical stability and solubility. Shikonin may be more stable and soluble in certain pH ranges, which can affect its absorption efficiency. Additionally, the presence of food in the GI tract can also influence shikonin absorption. Some components of food may interact with shikonin, either enhancing or inhibiting its absorption. For example, dietary fats may increase the absorption of lipophilic shikonin by facilitating its solubilization in the GI lumen.
3.2 Transporters and carriers
There are specific transporters and carriers in the body that can play a role in shikonin absorption. Identifying and targeting these transporters can be a strategy to enhance absorption. For instance, certain membrane transporters such as those belonging to the ABC transporter family may be involved in shikonin transport across epithelial cells. Modulating the activity of these transporters through the use of inhibitors or activators can potentially optimize shikonin absorption.

4. Distribution of shikonin
Once absorbed, shikonin is distributed throughout the body to reach its target sites.
4.1 Plasma protein binding
Shikonin can bind to plasma proteins such as albumin. Plasma protein binding affects the distribution of shikonin as only the unbound fraction is available for diffusion into tissues. Understanding the extent and nature of this binding is important for predicting shikonin's distribution. High - affinity binding to plasma proteins may limit its access to target tissues, while low - affinity binding may result in rapid clearance from the circulation. Strategies to modulate plasma protein binding can be explored to optimize distribution, such as the use of chemical modifications to shikonin to alter its binding affinity.
4.2 Tissue distribution
Shikonin has been shown to accumulate in certain tissues more than others. Its lipophilic nature may lead to preferential distribution into lipid - rich tissues such as adipose tissue. However, for its therapeutic applications, it is important to ensure adequate distribution to target tissues such as tumors or inflamed tissues. The use of targeted drug delivery systems, such as nanoparticles conjugated with ligands specific for target tissue receptors, can enhance the delivery of shikonin to the desired sites.
5. Metabolism of shikonin
Metabolism plays a crucial role in the fate of shikonin in the body.
5.1 Phase I metabolism
Phase I metabolic reactions, mainly carried out by cytochrome P450 enzymes in the liver, can modify shikonin. These reactions can include hydroxylation, oxidation, or reduction processes. The metabolites formed may have different biological activities compared to the parent compound. Some metabolites may be more active, while others may be less active or even inactive. Understanding the Phase I metabolism of shikonin can help in predicting its efficacy and potential toxicity. For example, if a metabolite is found to be more toxic, strategies can be developed to inhibit its formation.
5.2 Phase II metabolism
Phase II metabolism involves the conjugation of shikonin or its metabolites with endogenous molecules such as glucuronic acid or sulfate. This conjugation usually results in more water - soluble compounds, which are more easily excreted. However, the formation of certain Phase II metabolites may also affect the bioavailability of shikonin. For instance, if a highly water - soluble conjugate is rapidly excreted, it may reduce the overall exposure of the body to the active form of shikonin. Modulating Phase II metabolism through the use of enzyme inhibitors or inducers can be a strategy to optimize shikonin bioavailability.
6. Excretion of shikonin
The excretion of shikonin determines how long it remains in the body and its overall exposure.
6.1 Renal excretion
Renal excretion is an important route for the elimination of shikonin and its metabolites. The water - soluble metabolites formed during Phase II metabolism are predominantly excreted via the kidneys. Factors such as glomerular filtration rate and tubular secretion and reabsorption can influence the rate of renal excretion. For example, if tubular reabsorption of a shikonin metabolite is high, it may lead to a longer half - life of the compound in the body. Understanding these processes can help in optimizing dosing regimens to ensure effective elimination while maintaining therapeutic levels.
6.2 Hepatic excretion
Hepatic excretion, mainly through bile, also plays a role in shikonin elimination. Some shikonin metabolites may be excreted into the bile and then eliminated in the feces. The transport proteins involved in hepatic excretion can be targeted to enhance the elimination of shikonin. Additionally, drug - drug interactions that affect hepatic excretion should be considered, as certain drugs may compete for the same transport proteins and alter the excretion rate of shikonin.
7. Combination with other substances to improve bioavailability
Combining shikonin with other substances can be an effective strategy to enhance its bioavailability.
7.1 Co - administration with permeation enhancers
Permeation enhancers are substances that can increase the permeability of biological membranes. When co - administered with shikonin, they can help shikonin cross membranes more easily. For example, certain surfactants or fatty acids can disrupt the lipid bilayer of membranes, allowing shikonin to penetrate more efficiently. However, the safety and potential side effects of these permeation enhancers need to be carefully evaluated, as they may also affect the integrity of normal tissues.
7.2 Combination with drug carriers
Drug carriers such as liposomes and polymeric nanoparticles can be used to encapsulate shikonin. These carriers can protect shikonin from degradation, improve its solubility, and enhance its delivery to target tissues. Liposomes, for instance, are spherical vesicles composed of phospholipids that can mimic the cell membrane structure. Shikonin - loaded liposomes can fuse with cell membranes, facilitating the entry of shikonin into cells. Polymeric nanoparticles, on the other hand, can be designed with specific properties such as controlled release, which can prolong the exposure of the body to shikonin.
8. Advanced pharmaceutical techniques for optimizing bioavailability
Advanced pharmaceutical techniques offer new opportunities to improve the bioavailability of shikonin.
8.1 Nanotechnology - based formulations
Nanotechnology has revolutionized drug delivery. Nanoparticle formulations of shikonin can be engineered to have specific sizes, shapes, and surface properties. For example, nanoparticles with a size range of 1 - 1000 nm can take advantage of the enhanced permeability and retention (EPR) effect in tumors. This effect allows nanoparticles to preferentially accumulate in tumor tissues due to the leaky vasculature and poor lymphatic drainage in tumors. By formulating shikonin as nanoparticles, its delivery to tumors can be enhanced, thereby improving its bioavailability at the target site.
8.2 Microneedle - based delivery
Microneedle - based delivery systems are another innovative approach. Microneedles are small, micron - sized needles that can painlessly penetrate the skin. They can be used to deliver shikonin directly into the skin or underlying tissues. This bypasses the challenges associated with gastrointestinal absorption and first - pass metabolism. Shikonin can be incorporated into microneedle arrays, which can then be applied to the skin for controlled and efficient delivery.
9. Conclusion
In conclusion, optimizing the bioavailability of shikonin is a multi - faceted challenge that requires a comprehensive understanding of its chemical structure, absorption, distribution, metabolism, and excretion processes. By considering factors such as solubility, permeability, plasma protein binding, and the use of advanced pharmaceutical techniques and combination with other substances, it is possible to enhance the bioavailability of shikonin. This will ultimately enable the full realization of its therapeutic potential in the treatment of various diseases, including cancer, inflammation, and bacterial infections.
FAQ:
Question 1: What is shikonin?
Shikonin is a natural compound that has shown great potential in medicine due to its various biological functions, such as anti - inflammatory, anti - tumor, and antioxidant properties.
Question 2: Why is bioavailability important for shikonin?
Bioavailability is crucial for shikonin because it determines the extent to which the compound can be absorbed, distributed, metabolized, and excreted in the body. Limited bioavailability can restrict its full - scale application in medicine.
Question 3: How does the chemical structure of shikonin affect its bioavailability?
The chemical structure of shikonin can influence its solubility, permeability, and stability, which are all factors related to bioavailability. For example, certain structural features may limit its ability to cross cell membranes or be metabolized by the body.
Question 4: What are some methods to improve shikonin's absorption?
One method to improve shikonin's absorption is by formulating it with substances that enhance solubility or permeability. Another approach could be to use nano - technology to modify its particle size and surface properties, which may increase its uptake by cells.
Question 5: How can combination with other substances improve shikonin's bioavailability?
Combination with other substances can improve shikonin's bioavailability in several ways. For example, some substances can act as carriers to transport shikonin more effectively in the body. Others may inhibit enzymes that metabolize shikonin, thereby increasing its levels in the bloodstream.
Related literature
- Enhancing the Bioavailability of Shikonin: A Review of Current Strategies"
- "The Role of Pharmaceutical Techniques in Optimizing Shikonin Bioavailability"
- "Shikonin Bioavailability: Insights from Chemical Structure and Metabolism"
- ▶ Hesperidin
- ▶ citrus bioflavonoids
- ▶ plant extract
- ▶ lycopene
- ▶ Diosmin
- ▶ Grape seed extract
- ▶ Sea buckthorn Juice Powder
- ▶ Beetroot powder
- ▶ Hops Extract
- ▶ Artichoke Extract
- ▶ Reishi mushroom extract
- ▶ Astaxanthin
- ▶ Green Tea Extract
- ▶ Curcumin Extract
- ▶ Horse Chestnut Extract
- ▶ Other Problems
- ▶ Boswellia Serrata Extract
- ▶ Resveratrol Extract
- ▶ Marigold Extract
- ▶ Grape Leaf Extract
- ▶ blog3
- ▶ blog4
-
The best lemon juice powder in nature.
2024-12-01
-
Organic Vitamin K2 Powder Suppliers
2024-12-01
-
Bulk purchase of L - tyrosine.
2024-12-01
-
Vitamin K2 Manufacturers
2024-12-01
-
100% Pure Natural Rutin.
2024-12-01
-
Chinese Citrus Bioflavonoid Suppliers.
2024-12-01
-
Curcumin
2024-12-01
-
Ginger Extract
2024-12-01
-
Citrus Aurantii Extract
2024-12-01
-
Phyllanthus Emblica Extract
2024-12-01
-
Sea buckthorn oil
2024-12-01
-
Astaxanthin
2024-12-01
-
Acerola Juice Powder
2024-12-01
-
Lemon Juice Powder
2024-12-01
-
Aminolevulinic acid
2024-12-01
-
Peppermint Extract Powder
2024-12-01