- 0086-571-85302990
- sales@greenskybio.com
Scientific Studies on Cannabis for AS: Evaluating the Evidence for Pain and Inflammation Relief
2024-07-19
1. Introduction
Ankylosing Spondylitis (AS) is a chronic inflammatory disease that primarily affects the spine and sacroiliac joints. The symptoms of AS, such as pain, stiffness, and reduced mobility, can have a significant impact on the quality of life of patients. Cannabis, a plant with a long history of human use, has recently emerged as a potential treatment option for various medical conditions, including AS. However, its use remains controversial due to legal, social, and ethical considerations. This article aims to review the scientific evidence regarding the use of cannabis for pain and inflammation relief in AS patients.
2. The Chemical Components of Cannabis
Cannabis contains over 100 different cannabinoids, along with flavonoids, terpenes, and other compounds. The two most well - known cannabinoids are delta - 9 - tetrahydrocannabinol (THC) and cannabidiol (CBD).
2.1 Delta - 9 - Tetrahydrocannabinol (THC)
THC is the primary psychoactive component of cannabis. It binds to the cannabinoid type 1 (CB1) receptors, which are predominantly located in the central nervous system. Activation of CB1 receptors by THC can produce a range of effects, including pain relief, relaxation, and altered mood. However, THC also has potential side effects, such as dizziness, dry mouth, and cognitive impairment.
2.2 Cannabidiol (CBD)
CBD is a non - psychoactive cannabinoid. It has been shown to have anti - inflammatory, analgesic, and anxiolytic properties. CBD interacts with multiple receptors in the body, including the cannabinoid type 2 (CB2) receptors, which are mainly found in the immune system. By modulating the activity of CB2 receptors, CBD may help to reduce inflammation and pain in AS patients.
3. How Cannabis Interacts with the Body's Systems Relevant to AS Symptoms
The endocannabinoid system (ECS) plays a crucial role in maintaining homeostasis in the body. The ECS consists of endocannabinoids, cannabinoid receptors (CB1 and CB2), and enzymes that synthesize and degrade endocannabinoids. In AS patients, the ECS may be dysregulated, leading to increased inflammation and pain.
3.1 Interaction with the Endocannabinoid System
When cannabis is consumed, its cannabinoids can interact with the ECS. THC binds to CB1 receptors, mimicking the action of endocannabinoids. This can lead to a reduction in pain perception by modulating the activity of neurons in the pain pathways. CBD, on the other hand, can enhance the activity of endocannabinoids by inhibiting their degradation or by modulating the expression of cannabinoid receptors.
3.2 Anti - Inflammatory Effects
Cannabis has been shown to have anti - inflammatory effects through multiple mechanisms. CBD, in particular, can modulate the immune system by reducing the production of pro - inflammatory cytokines, such as tumor necrosis factor - alpha (TNF - α) and interleukin - 1β (IL - 1β). These cytokines are known to play a key role in the pathogenesis of AS. By reducing their levels, CBD may help to dampen the inflammatory response in AS patients.
3.3 Analgesic Effects
The analgesic effects of cannabis are thought to be mediated by both its interaction with the ECS and its anti - inflammatory properties. THC and CBD can act on different pain pathways in the body, including the peripheral and central nervous systems. They can also interact with other neurotransmitter systems, such as the opioid system, to enhance pain relief.
4. Scientific Studies on Cannabis for AS
Several scientific studies have been conducted to investigate the potential use of cannabis for AS.
4.1 Pre - clinical Studies
- Animal models: In animal models of AS - like inflammation, cannabis extracts or cannabinoids have shown promising results. For example, in a mouse model of ankylosing spondylitis, CBD treatment was associated with a reduction in joint inflammation and pain - related behaviors. The study suggested that CBD may act by suppressing the activation of immune cells in the joints.
- In vitro studies: In vitro studies using human cell lines have also provided insights into the mechanisms of action of cannabis in AS. For instance, CBD has been shown to inhibit the production of inflammatory mediators in cultured synovial cells from AS patients. These findings support the anti - inflammatory potential of CBD in AS.
4.2 Clinical Studies
- Small - scale clinical trials: Some small - scale clinical trials have been conducted to evaluate the efficacy of cannabis - based medications in AS patients. One study found that a combination of THC and CBD was associated with a significant reduction in pain and improvement in sleep quality in AS patients. However, the study had a small sample size and a short - term follow - up, limiting its generalizability.
- Observational studies: Observational studies have also reported on the use of cannabis for AS. A large - scale observational study found that a significant number of AS patients were using cannabis for pain relief. However, these studies are subject to confounding factors, such as the use of other medications and lifestyle factors.
5. Limitations of Current Studies
Despite the promising results from some studies, there are several limitations to the current scientific evidence on cannabis for AS.
5.1 Methodological Issues
- Small sample sizes: Many of the clinical studies on cannabis for AS have small sample sizes, which may limit the statistical power of the studies and make it difficult to draw definitive conclusions.
- Lack of control groups: Some studies lack appropriate control groups, making it difficult to determine whether the observed effects are truly due to cannabis or other factors.
- Short - term follow - up: Most of the studies have short - term follow - up periods, which may not be sufficient to evaluate the long - term safety and efficacy of cannabis for AS.
5.2 Heterogeneity of Cannabis Products
- Variable cannabinoid content: Cannabis products can vary widely in their cannabinoid content, including the ratio of THC to CBD. This heterogeneity makes it difficult to compare the results of different studies and to standardize the dosage of cannabis for AS patients.
- Delivery methods: Different delivery methods of cannabis, such as smoking, vaping, and oral ingestion, can also affect the bioavailability and pharmacokinetics of cannabinoids. This further complicates the evaluation of the efficacy and safety of cannabis for AS.
6. Potential Risks and Side Effects of Cannabis Use in AS
While cannabis may have potential benefits for AS patients, it also has potential risks and side effects.
6.1 Psychoactive Effects
THC, the psychoactive component of cannabis, can cause a range of mental effects, including euphoria, sedation, and cognitive impairment. These effects may be undesirable for some AS patients, especially those who need to maintain their mental clarity and functionality.
6.2 Respiratory Problems
Smoking cannabis can cause respiratory problems, such as coughing, wheezing, and bronchitis. These risks are similar to those associated with smoking tobacco. For AS patients who may already have respiratory complications due to their disease, smoking cannabis may pose an additional health risk.
6.3 Drug Interactions
Cannabis can interact with other medications that AS patients may be taking. For example, it can potentiate the effects of opioids, increasing the risk of overdose. It can also interact with immunosuppressive drugs, which are commonly used in AS treatment, potentially affecting their efficacy.
7. Conclusion
In conclusion, while there is some scientific evidence to suggest that cannabis may have potential for pain and inflammation relief in AS patients, the current evidence is limited by methodological issues and the heterogeneity of cannabis products. Future research should focus on conducting large - scale, well - designed clinical trials with long - term follow - up to better evaluate the safety and efficacy of cannabis for AS. Additionally, more research is needed to understand the mechanisms of action of cannabis in AS and to develop standardized cannabis - based medications. Until more conclusive evidence is available, the use of cannabis for AS should be carefully considered, taking into account the potential risks and side effects.
FAQ:
What are the main chemical components in cannabis relevant to AS?
Cannabis contains several chemical components, such as cannabinoids. Two of the most well - known cannabinoids are delta - 9 - tetrahydrocannabinol (THC) and cannabidiol (CBD). THC has psychoactive effects, while CBD is non - psychoactive. These cannabinoids may interact with the endocannabinoid system in the body, which is involved in various physiological processes relevant to AS symptoms, including pain perception and inflammation regulation.
How does cannabis interact with the body's systems related to AS?
The endocannabinoid system in the body has receptors that can bind to cannabinoids from cannabis. CB1 receptors are mainly found in the central nervous system, and CB2 receptors are more prevalent in the immune system and peripheral tissues. When cannabinoids interact with these receptors, they can potentially modulate neurotransmitter release, immune responses, and inflammatory pathways. In the context of AS, this interaction may lead to a reduction in pain and inflammation, as these processes are dysregulated in the disease.
What evidence exists from scientific studies regarding cannabis for pain relief in AS?
Some scientific studies have shown that cannabinoids may have analgesic (pain - relieving) effects. In animal models of AS - like conditions, treatment with cannabinoids has been associated with a reduction in pain - related behaviors. However, in human studies, the evidence is more limited. Some small - scale clinical trials and patient surveys have reported that patients with AS who use cannabis or cannabis - based products subjectively experience less pain. But more large - scale, well - controlled clinical trials are needed to firmly establish the efficacy of cannabis for pain relief in AS.
Is there evidence for cannabis reducing inflammation in AS?
Research has suggested that cannabinoids may have anti - inflammatory properties. In vitro studies have shown that cannabinoids can modulate the activity of immune cells involved in inflammation. In some pre - clinical models related to AS, treatment with cannabinoids has been associated with a decrease in inflammatory markers. However, translating these findings to humans with AS remains challenging, and more research is required to determine the true impact of cannabis on inflammation in the context of AS.
What are the potential risks of using cannabis for AS?
Using cannabis for AS also comes with potential risks. The psychoactive effects of THC can cause cognitive and psychological side effects, such as impaired concentration, memory problems, and in some cases, anxiety or paranoia. There may also be potential long - term effects on the respiratory system if cannabis is smoked. Additionally, the use of cannabis may interact with other medications that patients with AS are taking, potentially leading to adverse drug - drug interactions.
Related literature
- Cannabinoids in Ankylosing Spondylitis: A Review of the Current Evidence"
- "The Endocannabinoid System and Ankylosing Spondylitis: Potential Therapeutic Targets"
- "Cannabis - Based Therapies for Pain and Inflammation in Autoimmune Diseases: Focus on Ankylosing Spondylitis"
- ▶ Hesperidin
- ▶ citrus bioflavonoids
- ▶ plant extract
- ▶ lycopene
- ▶ Diosmin
- ▶ Grape seed extract
- ▶ Sea buckthorn Juice Powder
- ▶ Beetroot powder
- ▶ Hops Extract
- ▶ Artichoke Extract
- ▶ Reishi mushroom extract
- ▶ Astaxanthin
- ▶ Green Tea Extract
- ▶ Curcumin Extract
- ▶ Horse Chestnut Extract
- ▶ Other Problems
- ▶ Boswellia Serrata Extract
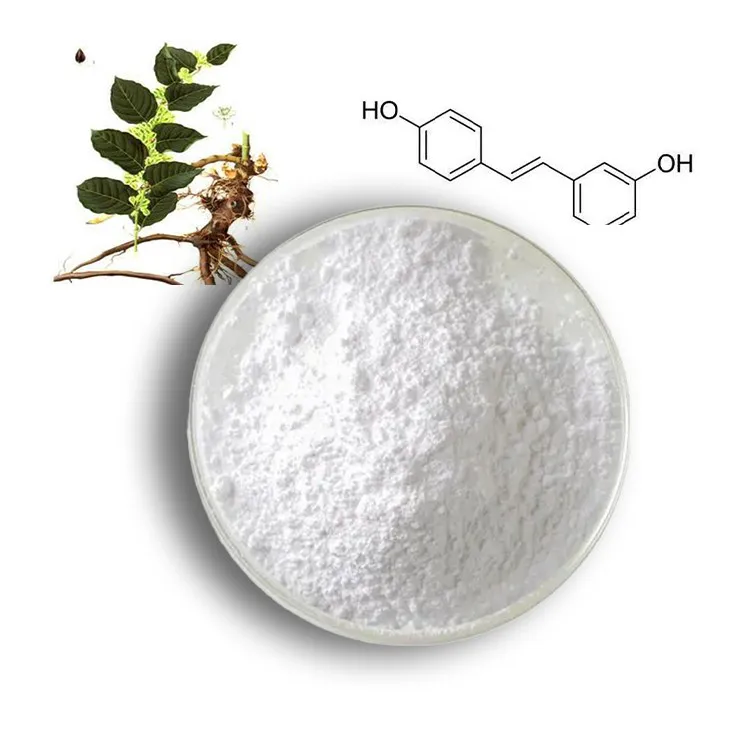
- ▶ Resveratrol Extract
- ▶ Marigold Extract
- ▶ Grape Leaf Extract
- ▶ blog3
- ▶ blog4
- ▶ blog5
-
Eyebright Extract
2024-07-19
-
Andrographis Paniculata Extract Powder
2024-07-19
-
Cassia Seed Extract
2024-07-19
-
Milk Thistle Extract
2024-07-19
-
Astaxanthin
2024-07-19
-
Motherwort Extract
2024-07-19
-
Sea buckthorn Juice Powder
2024-07-19
-
Saponin Extract
2024-07-19
-
Resveratrol extract
2024-07-19
-
Eucommia Ulmoides Extract
2024-07-19